Fertility treatments|Knowledge
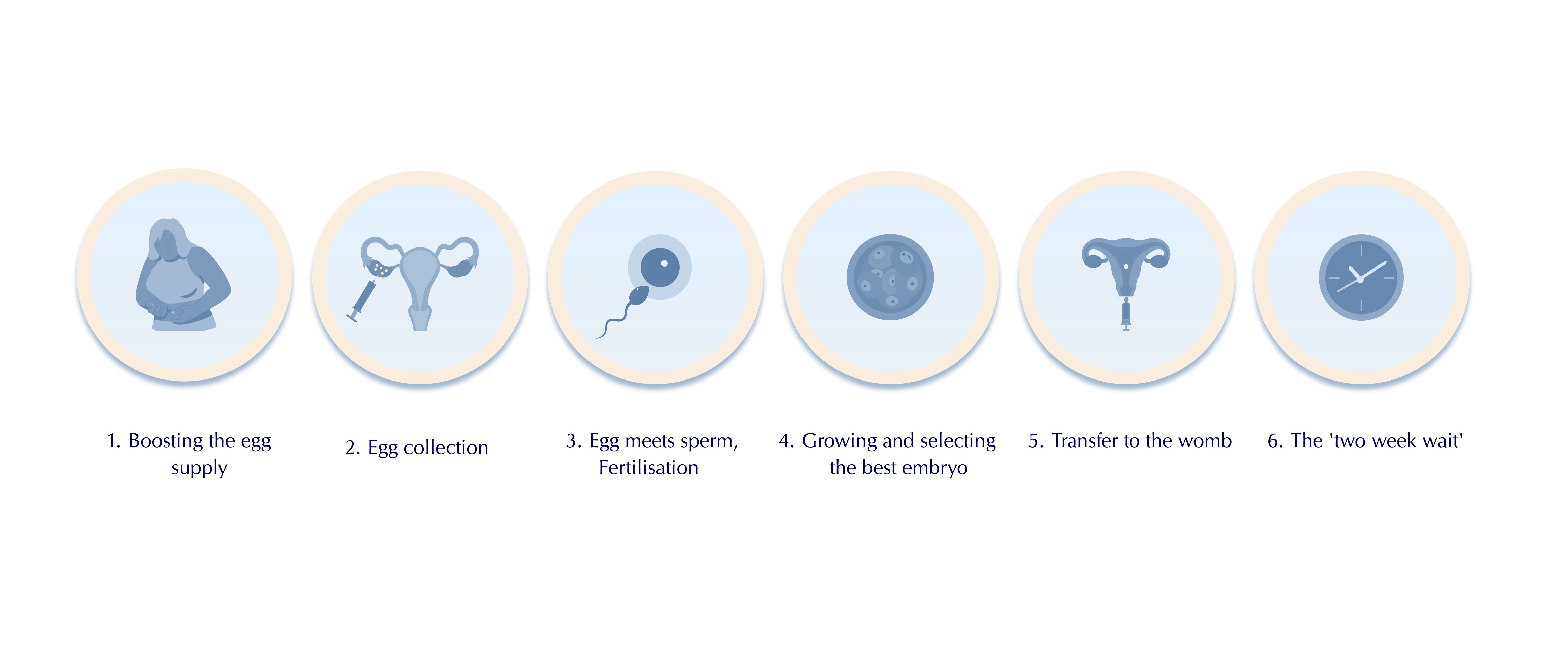
The IVF process: A step-by-step guide
Whether you’re considering starting your first IVF cycle or exploring other options to grow your family, the world of reproductive medicine might appear complex and overwhelming.
In this article, we break down the stages and timeline of IVF, so you have a clear understanding of what to anticipate if you choose this treatment on your journey to parenthood.
IVF Timeline: What to expect
Consultation with a Reproductive Endocrinologist and Infertility Specialist (REI)
Before beginning IVF treatment, you’ll meet with a fertility doctor, called a reproductive endocrinologist and infertility specialist, or REI for short. REIs are obstetrician-gynecologists with specialized training in treating infertility. Average wait times to see an REI varies from clinic to clinic, but can be up to six weeks.
At the first consultation, an REI will ask you a series of questions about your medical and family history and reproductive health to start determining the underlying cause of your struggle to conceive. Next, they will order lab tests to diagnose the cause of infertility.
Your REI may also order genetic screening for you and your partner. Carrier screening is a genetic test designed to determine if you carry genes associated with specific genetic disorders. This is typically done prior to or during pregnancy which will provide insights into the likelihood of your child inheriting a genetic disorder.
If your clinic is partnered with LEVY Health, the pre-screening process happens while you’re waiting for the first consultation, cutting up to 3 months of wait time off your fertility journey so you can begin your treatment much quicker.
You’ll answer questions about your health background at home via the virtual Reproductive Health Assessment. Once that’s done (it takes about 15 minutes), you’ll receive a lab requisition form that you can take to any Labcorp or Quest site near you for testing.
With your test results explained inside our digital dashboard and educational content about fertility in LEVY Learn, you can arrive at your first appointment at the clinic empowered with the knowledge of what’s been standing in the way of pregnancy and what questions to ask your doctor. That way, you can feel confident that you’re making the right decisions about your fertility treatment.
Ovarian stimulation cycle (8-14 days)
Now that all of the pre-screening and testing are out of the way, you’re all set to begin your IVF cycle. The first step of IVF is known as hormonal stimulation and involves taking hormonal medications daily. These medications make your ovaries produce multiple follicles, each potentially containing an egg.
Your dosage may change throughout this phase based on how your follicles are reacting and growing, which will be monitored at your clinic through regular ultrasounds and blood tests. Typically, ultrasounds occur on days 1, 5, 7, and 9 (and potentially additional ultrasounds as needed).

At the end of the stimulation cycle, you’ll have what’s known as a “trigger shot”. This is an injection of hormones (human chorionic gonadotropin or hCG) that helps your ovaries mature and release eggs so that they are ready for retrieval. The trigger shot happens 36 hours before your scheduled egg retrieval.
Egg Retrieval procedure (day 0)
On the day of egg retrieval, your partner will either provide a sperm sample, or you may already have frozen partner or donor sperm stored for use. The sperm will be “washed” (a process where an embryologist separates the highest quality sperm from lower quality sperm and semen to have higher chances of success) or thawed and prepared for intracytoplasmic sperm injection (ICSI).
To retrieve your eggs, you’ll receive anesthesia and your REI will use an ultrasound probe to guide a needle through your vagina and into one ovary at a time. The needle will then suck eggs and fluid from each follicle.
After retrieval, your eggs will go into an incubator (a device that helps maintain ideal atmospheric conditions for egg survival). An embryologist will examine each egg, remove cumulus cells (cells surrounding eggs that aid in maturation), and check its maturity
Eggs are graded in terms of maturity:
- GV = Germinal vesicle. These are the most immature eggs and will be discarded.
- MI = Metaphase I oocyte. These are immature eggs which may be kept for use during ICSI if there aren’t enough MII eggs. Some IVF labs don’t use MIs.
- MII = Metaphase II oocyte. These are mature eggs and have the highest chances for successful fertilization.
Around 4 hours following egg retrieval, an embryologist will perform ICSI. During ICSI, an embryologist selects a single sperm and injects it directly into the egg.
At this point, you’ll get an update about your IVF cycle from either your doctor, nurse, or IVF lab.
1 day after egg retrieval
The day after egg retrieval, embryologists check to see if sperm has successfully fertilized an egg. You’ll get another update on this day.
3 days after egg retrieval
It’s been 72 hours now, and an embryologist will check on how your embryos are developing and give them each a grade. Some IVF labs do it differently and won’t check the embryos on day 3 to avoid disturbing them. Now, the embryos have hopefully divided into 6, or preferably 8 cells. The more they’ve divided, the higher the chances for pregnancy.
You’ll get another update from your clinic on how things are moving along.
5 days after egg retrieval
This step of IVF is known as the blastocyst stage. It’s where a fertilized egg becomes a rapidly dividing ball of cells. The inner group of cells is the embryo and the outer group of cells nourishes and protects it.
An embryologist will evaluate and grade the embryos, likely using the most common and universally used grading system, called The Gardner Blastocyst Grading System:
- Expansion Stage: Grades 1 to 6
- 1-3 are the earliest developmental stages. An embryo must be at least a 3 to qualify for a biopsy, which is part of preimplantation genetic testing.
- 4-5 means that the blastocyst has “hatched.” This is when the blastocyst sheds its outer cellular membrane and it’s a necessary step for implantation.
- 6 is the most developed (fully hatched) stage.
- Trophectoderm (TE): Grades A to C
The trophectoderm is the collection of cells that will eventually become the placenta and pregnancy sac (fluid surrounding the embryo during the first few weeks). They are responsible for implantation of the embryo into the wall of the uterus.
- A means there are lots of cells (which is what you want).
- B means there are fewer cells.
- C is the lowest, meaning there are the least cells.
- Inner Cell Mass (ICM): Grades A to C
The inner cell mass is a mass of cells within the blastocyst which will turn into the fetus.
- A means there are many tightly packed cells (which is the best grade).
- B means that there are many loosely grouped cells.
- C means that there are very few cells.
If you’re having a fresh embryo transfer, the embryo with the best grade across all 3 categories will be transferred into your uterus on day 5. If you’re doing preimplantation genetic testing (PGT), an embryologist will take a biopsy of the additional viable embryos and then freeze them for a future frozen embryo transfer (FET).
6 days after egg retrieval
If any of your embryos haven’t reached the blastocyst stage on day 5, an embryologist will check and grade them on day 6. Like on the previous day, any embryos that will go through preimplantation genetic testing will undergo a biopsy and then get frozen. You’ll receive an update from your doctor about how your embryos are developing.
7 days after egg retrieval
Depending on your IVF lab, an embryologist may check the embryos one last time to see if any more have advanced to the blastocyst stage. Not all labs give embryos until the 7th day to develop. Like the last step, any viable embryos that advanced to day 7 will be biopsied and frozen and you’ll get an update on the progress.
Embryo transfer
Once the embryos are developed enough, they can be transferred into your uterus. Your REI will insert a catheter (a thin tube) through your vagina and cervix and into your uterus to release the embryo.
Two weeks wait
If the embryo successfully implants itself in the uterine wall, which may take around 6 to 14 days, you’ll become pregnant. You’ll need to return to your fertility clinic for a blood test to confirm the pregnancy.
Takeaway
IVF is an effective fertility treatment and offers hope for many aspiring parents dealing with infertility. Remember, each IVF journey is unique, and success rates can vary based on numerous factors, including age and underlying fertility issues.
While it is a complex process and can feel overwhelming at times, we hope that now that you know how IVF works you have more clarity as you embark on the next step of your fertility journey.
Don’t hesitate to reach out to your clinic for help with questions you have along the way and emotional support as you navigate the world of fertility treatment. Try not to get discouraged if the outcome isn’t one you were hoping for the first time around – it’s common for IVF to need multiple cycles to lead to a successful and healthy pregnancy.
This article has been verified by a medical professional.
In Vitro Fertilization (IVF). Healthline. Accessed 17 January 2024.
Genetic Carrier Screening. Johns Hopkins Medicine. Accessed 17 January 2024.
ICSI Sperm Prep. Ovation Fertility. Accessed 17 January 2024.
IVF embryo quality and day 3 embryo grading after in vitro fertilization Cleavage stage embryo grading. Advanced Fertility Center of Chicago. Accessed 17 January 2024.
Blastocyst. Mayo Clinic. Accessed 17 January 2024.
Cochrane Gynaecology and Fertility Group et al.: “Day 5 versus day 3 embryo biopsy for preimplantation genetic testing for monogenic/single gene defects.” Cochrane Database Syst Rev. 2022;2022(11): CD013233.
Blastocyst. Cleveland Clinic. Accessed 17 January 2024.
You might also like...
Female hormones: What you need to know about reproductive hormones, the menstrual cycle, and fertility
When you’re struggling with fertility, one of the first places to look is your hormones. Certain vital reproductive hormones are in charge...
Silvia Hecher
January 17, 2024
Fertility blood test: Why does it need to be cycle days 2-5?
When you test your fertility with LEVY, you will always check your basic reproductive hormone levels (including FSH, LH, TSH, Prolactin, Estradiol,...
Lena
September 8, 2022

Forms of amenorrhea and fertility
Not getting your period is a condition called amenorrhea. It’s important for fertility because not having a menstrual cycle with monthly ovulation...
Lena
January 18, 2022

Fertility Foods for Women to Help You Get Pregnant Faster
How you nourish your body is key not only when you have a baby in your belly, but also to help prepare...
Kayla
March 22, 2022

10 Reasons IVF can fail and What to Do Next
Why IVF fail: Although in-vitro fertilization (IVF) can help many people who weren’t able to conceive naturally have a child, there’s unfortunately...
Lena
March 2, 2023
Iron: The secret ingredient for fertility?
Getting your daily recommended amount of vitamins and minerals is key to getting pregnant and having a healthy pregnancy. So, how does...
Lena
November 30, 2022
What your AMH levels can tell you about fertility
FSH, LH, estrogen, progesterone… If you’re struggling to have a baby, you’re probably becoming an expert on all things hormones. AMH is...
Lena
August 25, 2022

6 Interesting Facts About Ovaries You Might Not Know
Women have two ovaries which are located on either side of the uterus. They’re around 3-5 cm long – about the size...
Kayla
April 20, 2022

What to expect when testing your fertility with LEVY
If you’ve been trying to conceive for a while, it’s totally normal to feel frustrated. Why hasn’t it happened for you yet,...
Kayla
February 3, 2022




