Knowledge
Antiphospholipid Syndrome (APS)
Antiphospholipid syndrome (APS), also known as Hughes syndrome, is an autoimmune disease that increases someone’s risk for developing blood clots. In this condition, the body’s immune system mistakenly creates antibodies which attack phospholipids. These are proteins attached to fat molecules and play an important role in blood clotting. When phospholipids get destroyed it can create bleeding problems, causing clotting or an increased tendency to bleed (thin blood). APS matters for fertility because bleeding problems can cause miscarriage, premature birth and other pregnancy complications.
Studies show that up to 5% of the population are APLA-positive, meaning they have antibodies for phospholipids in their blood. But not everyone with these antibodies experiences symptoms. Women develop the disease much more frequently than men (3 to 5 times more), often already in the mid-20s – pretty bad timing when you’re trying to have children. Experts aren’t sure what causes someone to develop APS.
How do you know you have antiphospholipid syndrome (APS)?
The main symptom of antiphospholipid syndrome is blood clots. When a blood clot blocks a vein, it’s known as thrombosis. Thromboses happen most often in the legs.
Symptoms of a thrombosis in the leg include:
- Throbbing and cramping in the calf or thigh of one leg
- Swelling in one leg
- Warm, red, or dark skin around the painful area
- Swollen veins
When a blood clot forms in an artery, it’s called an embolism. These usually occur in the brain and can lead to a stroke.
Antiphospholipid syndrome (APS) & miscarriage
APS is the most common, treatable cause of recurrent miscarriage (15% are due to APS), but it can also cause other types of complications during pregnancy. Antiphospholipid antibodies lead to early pregnancy loss because they stop the embryo from properly implanting in the uterus and stop fetal cell growth. The majority of miscarriages in women with APS happen in the first 13 weeks of pregnancy.
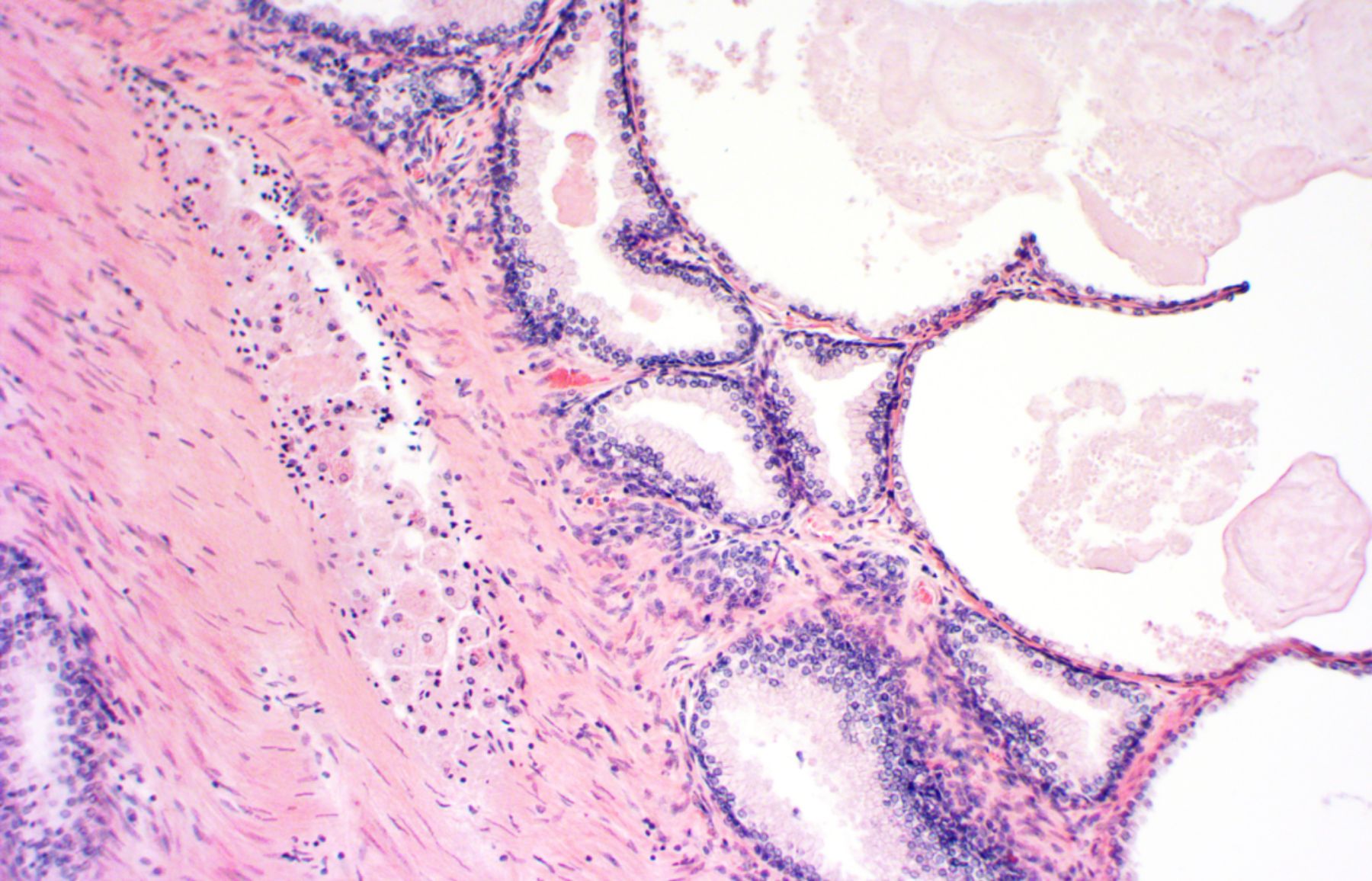
Late pregnancy loss is also common in women with APS, with miscarriage occuring between three and six months. Antibodies cause clots in the small veins of the placenta. This prevents the placenta from supplying the baby with the nutrients and oxygen necessary to grow.
How is antiphospholipid syndrome (APS) diagnosed?
Symptoms of APS alone aren’t enough to diagnose the condition, because they can be caused by other health problems. So doctors need to perform tests in order to definitively diagnose APS and detect antibodies in the blood.
In 2006, an expert panel came up with the following clinical criteria to diagnose APS:
1) Blood clots
One or more blood clots confirmed by an imaging scan or examination of tissue samples.
2) Pregnancy complications
- One or more unexplained late miscarriage at or after week 10 of pregnancy.
- One or more premature births at or before the 34th week of pregnancy, either due to severe preeclampsia, eclampsia or placental insufficiency.
- Three or more unexplained early miscarriages before 10 weeks of pregnancy that aren’t due to chromosomal abnormalities or a hormonal imbalance.
Lab criteria
Two irregular lab results tested at least 12 weeks apart:
- Elevated levels of anticardiolipin antibodies in the blood.
- Detection of lupus anticoagulants in blood plasma.
- Elevated anti-beta-2-glycoprotein-1 antibodies.
Find out if you may have APS with the LEVY Fertility Code:
How is APS treated?
Treatment for APS aims to reduce the risk of blood clots, and is successful at reducing the risk for pregnancy complications. With correct diagnosis and treatment, the APS Support UK Foundation cites that the pregnancy success rate of people with APS has risen from 20% pre-1990 to around 70-80% today.
Most people with APS are prescribed an anticoagulant or antiplatelet medication, to take daily for the rest of their life. But for people without a history of blood clots, doctors usually recommend low-dose aspirin tablets.
Be sure to tell your doctor that you are trying to get pregnant so they can take this into account when making your dosage and prescription. Treatment during pregnancy usually involves taking a daily dose of aspirin and/or heparin. Studies show that combining the two reduces the risk of having another miscarriage for women who previously had a pregnancy loss.
There are also certain lifestyle changes you can make to reduce your chance of getting blood clots, including:
- Quit smoking if you are a smoker (which is also very important when trying to conceive!)
- Eat a healthy, balanced diet (check out our article on female fertility diets)
- Exercise regularly
- Lose weight if you are overweight or obese
For more advice on having a healthy pregnancy, take a look at our article: 9 Tips to Prepare for Pregnancy.
Takeaway
Antiphospholipid syndrome (APS) is an autoimmune disorder that increases the risk of blood clots. It matters for fertility because APS is the most common cause of recurrent miscarriages (having 3 or more miscarriages in a row). APS leads to pregnancy loss because it prevents an embryo from implanting properly in the womb and blocks the flow of oxygen and nutrients to the growing baby.
If you’ve had at least two miscarriages, don’t wait for the third one to get tested. Decode your fertility with LEVY to see what’s preventing you from having a successful pregnancy. We will get to the bottom of it in just a few weeks and create a custom action plan to help you along your path to parenthood.
DVT (deep vein thrombosis). NHS. Accessed 28 July 2022.
Pregnancy. APS Support UK. Accessed 28 July 2022.
Treatment Antiphospholipid syndrome (APS). NHS. Accessed 28 July 2022.
You might also like...
Female hormones: What you need to know about reproductive hormones, the menstrual cycle, and fertility
When you’re struggling with fertility, one of the first places to look is your hormones. Certain vital reproductive hormones are in charge...
Silvia Hecher
January 17, 2024
Fertility blood test: Why does it need to be cycle days 2-5?
When you test your fertility with LEVY, you will always check your basic reproductive hormone levels (including FSH, LH, TSH, Prolactin, Estradiol,...
Lena
September 8, 2022

Forms of amenorrhea and fertility
Not getting your period is a condition called amenorrhea. It’s important for fertility because not having a menstrual cycle with monthly ovulation...
Lena
January 18, 2022

6 Interesting Facts About Ovaries You Might Not Know
Women have two ovaries which are located on either side of the uterus. They’re around 3-5 cm long – about the size...
Kayla
April 20, 2022

What to expect when testing your fertility with LEVY
If you’ve been trying to conceive for a while, it’s totally normal to feel frustrated. Why hasn’t it happened for you yet,...
Kayla
February 3, 2022

Your Complete Guide to Birth Control Options and Fertility
If you’ve been using birth control for a while, you may be wondering how it can impact your fertility now that you...
Kayla
February 21, 2022

Fertility Foods for Women to Help You Get Pregnant Faster
How you nourish your body is key not only when you have a baby in your belly, but also to help prepare...
Kayla
March 22, 2022
What your AMH levels can tell you about fertility
FSH, LH, estrogen, progesterone… If you’re struggling to have a baby, you’re probably becoming an expert on all things hormones. AMH is...
Lena
August 25, 2022

Why Vitamin D matters for fertility
Vitamin D is a very important nutrient to keep our bodies healthy and working as they should. But did you know that...
Kayla
January 18, 2022




